Part 2
As discussed in Part 1 of this series, neuroinflammation – also known as “brain on fire” – is a common problem for those who have taken fluoroquinolones in the past. If you are experiencing symptoms ranging from brain fog to seizures, it’s essential to identify if your brain is inflamed.
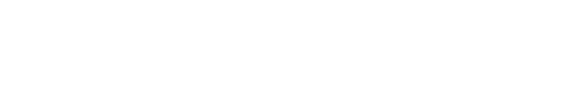
There are various tests available to determine neuroinflammation. One of the latest tests available measures blood brain barrier permeability. This test assesses the integrity of the membrane between your blood and brain, and detects if your blood brain barrier is leaking, allowing proteins to enter your bloodstream that shouldn’t be there.
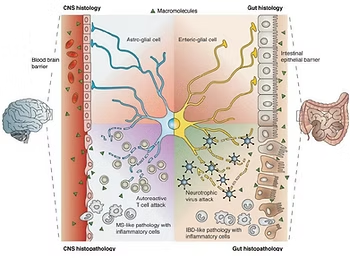
The Blood Brain Barrier Permeability Screen measures whether the level of specific proteins in the blood is “in range” or “out of range.” If the level is out of range, it indicates that the blood brain barrier is leaking, or starting to break down. Fluoroquinolones can damage the blood brain barrier since they are attracted to the fat tissue that makes up the brain. This damage causes inflammation because particles can enter your bloodstream where your immune system attacks them
Why Blood Brain Barrier is Susceptible to Damage
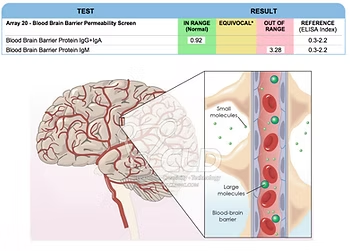
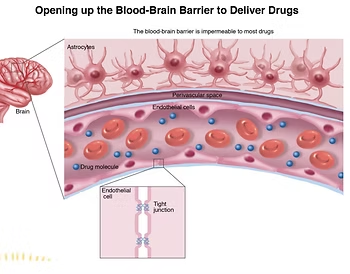
The blood brain barrier is only one cell thick, and this makes it more vulnerable to damage. In comparison, the skin on your fingertip consists of tens of thousands of cells, which creates a barrier between the outside world and your blood.
If the barrier between your bloodstream and brain is damaged, foreign substances can easily enter your brain.
Just like food sensitivities, where proteins in food permeate the one-cell lining of the intestines, causing inflammation, the blood brain barrier can be impacted by foreign substances. Once the blood brain barrier is damaged, it loses its impermeability, resulting in a leaky brain.
The Impact on Neurons
The above graphic shows an impermeable blood brain barrier compared to a leaky one. When fluoroquinolones destroy the blood brain barrier, they can directly pass into the brain once the barrier deteriorates. These chemicals can destroy the mitochondria of your neuronal cells, also known as the “power packs,” causing the cells to malfunction. Unlike other cells in the body, neurons cannot rebuild themselves after they’ve been damaged. Addressing the symptoms of neuroinflammation is crucial to protect your brain cells.
The Role of Glial Cells in the Brain
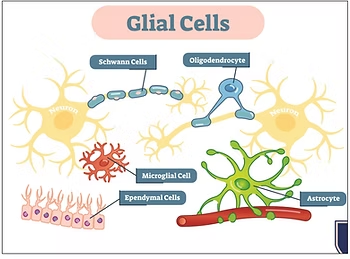
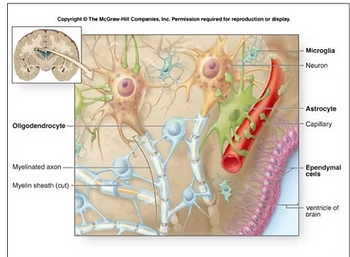
Research shows that neurons only make up about 10 percent of your brain’s cells, while the rest (90 percent) are called glial cells. These cells include Schwann cells, oligodendrocytes, microglial cells, ependymal cells, and astrocytes, and they have different roles in the brain
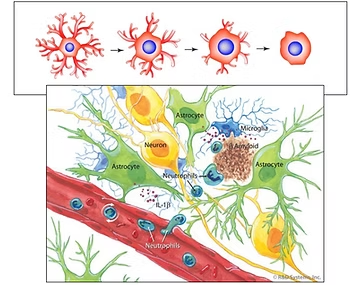
The essential function of glial cells is to support and protect neurons, acting as your brain’s immune system. When your immune system is compromised due to inflammation, glial cells mistakenly attack neurons, resulting in various symptoms.
Glial cells do far more than just hold neurons together. They have a range of functions, including regulating the body’s immune system and helping to form myelin, which is the insulation that surrounds neurons. When glial cells are inflamed, they can no longer perform these essential functions.
The goal of resolving neuroinflammation is to restore health to the glial cells. When the immune system is functioning correctly, it can target and eliminate harmful pathogens and toxins. This helps to reduce inflammation and promote the body’s healing process. A healthy immune system also helps to protect the brain from future damage caused by pathogens or toxins.
Conclusion
In conclusion, neuroinflammation, or “brain on fire,” is a common problem among individuals who have taken fluoroquinolones in the past. The Blood Brain Barrier Permeability Screen is one of the tests that can pinpoint neuroinflammation. It is also important to note the role of glial cells in the brain. Glial cells comprise many different types of brain cells and have essential functions, including supporting and protecting the neurons, regulating the body’s immune system, and forming myelin.
Frequently Asked Questions (FAQ)
It's a specialized test that measures specific proteins in the blood to determine if the blood-brain barrier is "leaky." An "out of range" result indicates the barrier is compromised, allowing inflammatory substances to enter the brain.
Unlike other cells, neurons cannot regenerate or rebuild themselves once they are damaged. This makes it crucial to identify and address neuroinflammation early to protect these vital cells.
Glial cells make up 90% of your brain and act as its immune system. When inflamed, they can mistakenly attack and damage neurons. The goal of treatment is to calm these glial cells to resolve inflammation and protect the brain.