To gain a deeper understanding of how your body functions in relation to others, examining laboratory test results can be invaluable. However, it’s crucial to comprehend the functional range for a normal, healthy individual and compare it with your own or someone who is sick or unhealthy. In the case of insulin, a hormone notorious for inducing inflammation, a fasting level between 5 and 7 is considered ideal for a healthy person. Keep in mind that when undergoing bloodwork, particularly for insulin levels, it is imperative to fast for 8 to 10 hours beforehand to avoid any interference from food-induced insulin spikes.
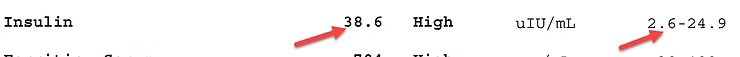
Let’s begin by discussing one of my clients who was experiencing significant health issues. His lab results revealed an insulin level of 38, a remarkably high figure that went unnoticed until then.
Knowing his insulin was so high, we can immediately assume he is experiencing some sort of severe, chronic inflammation. You may also notice that the range on this lab is 2.6 to 24.9. That is ridiculous, it is too broad. We want to narrow it down, and get it to a smaller, more normal range.
The conventional system overlooked this person’s blood work in this case. An insulin level of 38 is extremely high. There may be other markers you should consider, such as glucose level. Also examining other blood sugar markers in conjunction with insulin levels may point to sugar dysregulation.
Research Backs the Connection
A plethora of research and data supports the correlation between insulin and inflammation. Numerous articles have delved into this subject, with some offering comprehensive reviews backed by over 100 references. One notable study, titled “Type 2 Diabetes Mellitus and Alzheimer’s Disease: Role of Insulin Signaling and Therapeutic Implications,” was published in 2018. It revealed a correlation between type II diabetes, characterized by insulin resistance and elevated insulin levels, and the development of Alzheimer’s disease.
In their conclusion, the authors emphasized that insulin plays a vital role in brain function and highlighted the heightened risk of developing conditions such as Alzheimer’s disease, Parkinson’s disease, and neuroinflammation due to insulin imbalances. Therefore, monitoring insulin levels becomes even more crucial for those grappling with chronic health issues. Altered insulin metabolism, characterized by high insulin levels and impaired signaling, contributes to the onset and progression of these disorders by influencing the regulation of neural pathological hallmarks.
A Glimmer of Hope: Achieving Improvement
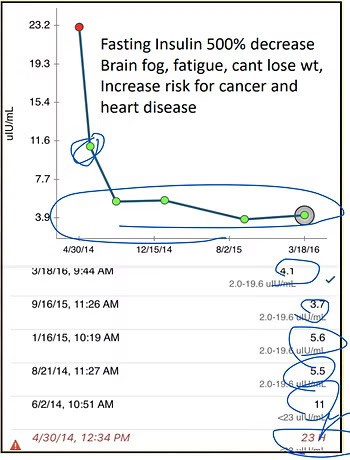
In essence, elevated insulin levels lead to impaired brain and body function, perpetuating chronic inflammation. Here’s an illustrative example from one of my patients. Initially, her insulin level stood at 23, but after implementing an insulin-control protocol and consistently monitoring her levels, they gradually decreased to 11, and eventually settled within the range of 3.7 to 5.6. These significant improvements demonstrated stabilization within the desired “sweet spot” for optimal health.
If you find yourself suffering from chronic problems, it is crucial to check your insulin levels. Early detection and proactive measures can help prevent further complications and improve your overall well-being.
Seeking Help and Finding Hope
If you found this information helpful, consider sharing it with those who may benefit from it. Remember, seeking help is the first step toward finding hope in your journey to combat chronic inflammation. Consult with a healthcare professional experienced in managing insulin levels to develop an individualized plan tailored to your specific needs. Together, we can work towards better health and a brighter future.
Video time stamps
[00:00:25] insulin is a hormone
[00:02:05] fasting insulin sweet spot 5 to 7 fasting
[00:03:10] super high 38
00:03:35] dysregulation insulin
[00:05:05] Type two diabetes and Alzheimer’s
[00:05:45] Increased risk for Alzheimer’s, Disease, Parkinson’s disease and neuroinflammation.
[00:05:55] brain.
[00:06:15] High insulin means bad brain, bad body, chronic inflammation.
Frequently Asked Questions (FAQ)
High insulin levels are a significant problem because insulin is a hormone notorious for inducing severe, chronic inflammation. Elevated insulin can lead to impaired brain and body function and is linked to conditions like Alzheimer's disease and neuroinflammation.
A fasting insulin level between 5 and 7 uIU/mL is considered ideal for a healthy person. It's important to compare your results to this functional range rather than the broader standard lab range (e.g., 2.6-24.9), which can be too permissive.
Yes, significant improvement is possible. Through a targeted protocol, one patient's insulin level was successfully reduced from 23 uIU/mL to a stable, healthy range between 3.7 and 5.6 uIU/mL, demonstrating that it's possible to lower insulin and the chronic inflammation it causes.