In today’s busy, ever-connected world, more of us are admitting, “I just feel so foggy.” Have you ever felt engulfed by a mysterious haze clouding your thoughts? Or maybe you’re constantly drained, forgetting where you last left your favorite mug? Dive with me into the concept of a “leaky brain” and you might find the surprising answers linked to blood-brain barrier damage symptoms. Don’t worry; I’ve got you covered, explaining everything simply and clearly.
Understanding Blood Brain Barrier Permeability: A Peek into the Purple Box
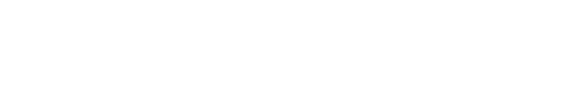
Imagine this scenario: a dear friend shows me her latest medical reports, searching for clarity. That intriguing purple section? It’s labeled the Blood Brain Barrier Permeability. In layman’s terms, think of it as the security system for your brain. Now, if there are two bold red arrows there flagging “out of range,” it’s a sign that there’s a leak in the security.
Your blood-brain barrier is akin to the walls of a fortress, incredibly thin – just one cell in width! When this barrier leaks, unwanted guests from your bloodstream, like inflammation, can waltz right into your brain. But here’s the twist: our brains don’t cry out in pain. Instead, it manifests as fatigue, forgetfulness, and even a sense of imbalance. Ring any bells?
Feeling foggy isn’t just a fleeting feeling. It’s a genuine sign that there might be an underlying issue. Ever been gripped by sudden anxiety? Or felt an inexplicable bout of sadness? These aren’t mere mood swings. They might be red flags hinting at blood-brain barrier damage symptoms.
Grasping the True Threat
This isn’t about minor forgetfulness. A compromised brain barrier is a grave concern. It means the defense mechanism of your brain has vulnerabilities. This isn’t just alarming, it’s an autoimmune condition that directly targets brain tissues.
Frequently Asked Questions (FAQ)
The most common symptoms are cognitive and emotional rather than painful. They include persistent brain fog, chronic fatigue, forgetfulness, a feeling of imbalance, sudden anxiety, and unexplained bouts of sadness. These are your brain's way of signaling that its security system is compromised.
It can be diagnosed with specific medical tests like the Array 20 Blood Brain Barrier Permeability test. This test measures antibodies (IgG and IgM) related to the barrier; results flagged as "out of range" with red arrows indicate a "leak" in the brain's security system.
It's a grave concern because it's not just minor forgetfulness—it's an autoimmune condition that directly targets brain tissue. A compromised barrier allows inflammation and other unwanted elements from the bloodstream to enter the brain, leading to significant neurological symptoms and dysfunction.